By: Katherine Record, Executive Director, Beth Israel Lahey Health Medicaid ACOs and Performance Network Compliance & Privacy Strategy, HFMA MA-RI Chapter, Compliance Committee Member,
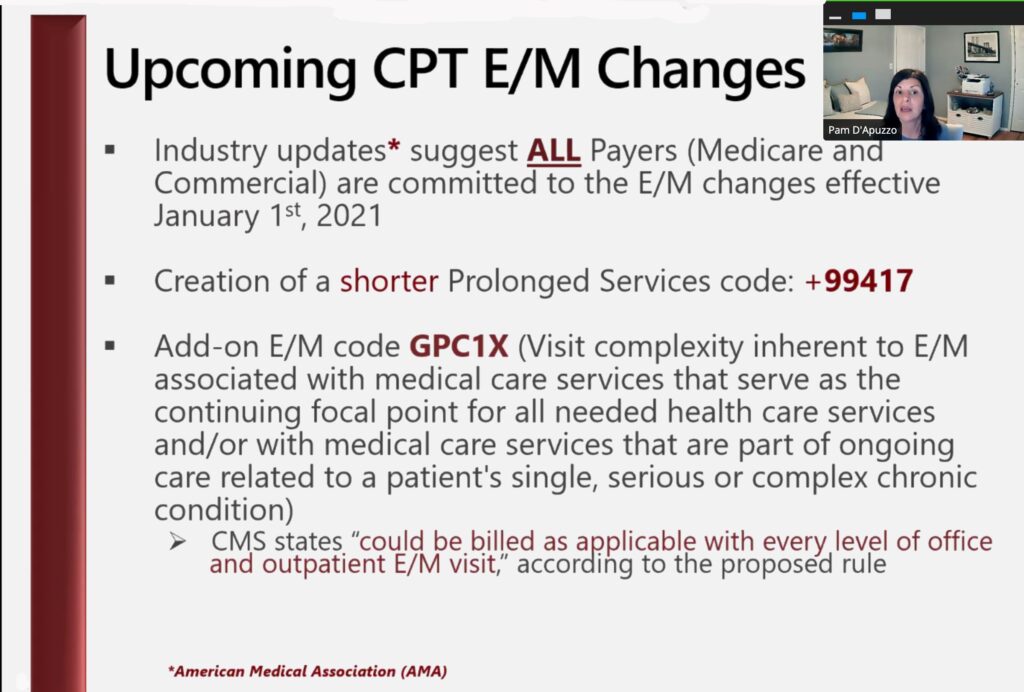
CMS is making changes to E/M codes 99201-99205 and 99211-99215, which are likely to be adopted universally across all payers (including commercial).
What do you need to know?
- For the first time, physical exam and history are not necessarily required to use these codes
- Providers no longer need to spend 50% or more of the visit on “counseling and coordinating care” (except if visit is occurring in a facility)
- Providers have more flexibility to bill for the actual amount of time they spend with patients (face to face or otherwise)
- Coding decisions are simplified, in that a provider can document time spent with a patient or level of Medical Decision Making (MDM) required
- Providers can factor social needs of patients into the level of MDM (e.g., a homeless patient may require more of the provider’s time as well be more clinically acute)
- Providers can utilize new codes for prolonged services (adding 15 minute increments onto visits) as well as for complex visits
- Provider teams can bill for “split time” on the same patient (e.g., if a nurse and physician are in the same room with a patient, both offering their services)
Thank you to Pam D’Apuzzo for very information presentation.
Click HERE for a copy of her presentation.